Legiolert*
For detection of Legionella pneumophila
![]()
![]()
![]()
- Legionella test for all serotypes of Legionella pneumophila with equal or greater accuracy than traditional spread plate culture methods.1-12
- Significantly improves Legionella testing workflow, leading to higher productivity.
- Liquid culture test; isolates can be stored and/or serotyped.
- Reports in MPN, equivalent to CFU per ISO 6107:2021.
- Specified as a recommended method in the Standing Committee of Analysts “Blue Book” publication.
- Received NF Validation by AFNOR Certification, reference number IDX 33/06-06/19.
Benefits
Easy
- Improved Legionella testing workflow for increased laboratory profitability.
- Less than 5 minutes of hands-on time compared to 10-40 minutes required for traditional spread plate methods.13
- Objective and easy-to-read results.
- No confirmation step required.
Accurate
- More resistant to competing non-Legionella organisms than traditional spread plate methods.1,2,7-9
- Demonstrated to be as or more sensitive than traditional spread plate methods in several independent, peer-reviewed studies. 1-4,6-12
- Highly specific for all serotypes of Legionella pneumophila, confirmed in several peer-reviewed studies.1-3,8-10,12
Accepted
- Used by public, utility, and private laboratories around the world.
- Included in the UK Standing Committee of Analysts’ Blue Book.
- Published by ASTM International as Standard D8429-21.
- Received NF Validation by AFNOR Certification, reference number IDX 33/06-06/19.
- Listed as bacterial enzyme culture method in ASHRAE Guideline 12.
Why test for Legionella pneumophila?
- Causes 100% of deaths from Legionnaires' disease outbreaks14-19
- Causes 97% of Legionnaires' disease cases, based on data from cultures of 4,719 patients over seven years in 17 countries20
- The only cause of Legionnaires' disease cooling tower outbreaks17-21
- Saves time and resources; eliminates unnecessary remediations for non-pneumophila species
Science
How the Legiolert Test works
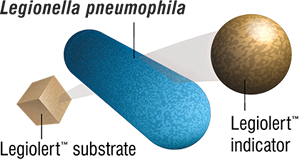
The Legiolert Test detects Legionella pneumophila in water samples. This test is based on a bacterial enzyme detection technology that signals the presence of Legionella pneumophila through utilisation of a substrate present in the Legiolert reagent. L.pneumophila cells grow rapidly and reproduce using the rich supply of amino acids, vitamins, and other nutrients present in the Legiolert reagent. Actively growing strains of L. pneumophila use the added substrate to produce a brown colour indicator. The Legiolert Test detects L. pneumophila at 1 organism in 100 mL within 7 days.
How to use
Learn how to use the Legiolert test
Potable protocols
Which potable protocol should I choose?
Potable (10mL protocol)
Potable (100mL protocol)
Nonpotable protocols
Nonpotable (1.0mL protocol)
Legiolert protocol steps
Frequently asked questions
General
Yes. Legiolert was granted NF Validation Certification by AFNOR in 2019 and is published as ASTM International Standard D8429-21. It is also included in the UK Standing Committee of Analysts Blue Book: The determination of Legionella bacteria in waters and other environmental samples (2020) – Part 2 – Culture Methods for the detection and enumeration and is referenced as a bacterial enzyme method in ASHRAE Guideline 12.
Legiolert has also been extensively compared to traditional methods of Legionella detection in several independent peer-reviewed studies. Please contact IDEXX Water Technical Services at EMEATechSupport@idexx.com for the most up to date list of publications.
Yes. The Legiolert test detects all serogroups of L. pneumophila. This was confirmed in the test’s ISO 13843 study, as well as an independent peer-reviewed study.5
Yes. Legiolert is a culture test and yields a viable isolate which can be serotyped and/or stored as necessary. IDEXX has developed and validated a procedure for serotyping directly from a positive well, which eliminates the need to subculture from positive wells. Please contact IDEXX Water Technical Services at EMEATechSupport@idexx.com for this procedure.
No. All microbiological methods have some rate of false positivity. Although the false positive rate of traditional spread plate methods of Legionella detection has not been well studied, false positives have been demonstrated in those methods.26 In contrast, the Legiolert test’s rate of false positivity in environmental samples has been well studied, and has been demonstrated to be very low in several independent peer-reviewed studies, between 0 and 4%.1-3,8-10,12
Legiolert can be used globally for any Legionella testing outside the context of a specific regulation. Legiolert can always be used for any non-compliance testing to reduce risks associated with Legionnaires’ disease.
Additionally, the Legiolert test is currently being considered as an alternate method for several regulations around the world. Please contact IDEXX Water Technical Services at EMEATechSupport@idexx.com for the most recent status or approvals.
Technical
The Legiolert test is designed specifically for potable and nonpotable water samples.
Potable water is water that is fit for consumption and includes hot and cold water from kitchen or bathroom taps, showers, or water within a drinking water distribution system, among others.
Nonpotable water is not fit for consumption and includes water from cooling towers, pools, spas, decorative fountains, among others.
Please contact IDEXX Water Technical Services at EMEATechSupport@idexx.com if you need assistance classifying your water sample.
Yes, the Legiolert potable and nonpotable protocols have each been designed for optimal performance with different types of water. Testing a nonpotable sample with the potable protocol may provide false-positive results due to bacteria other than L. pneumophila. Testing a potable sample with the nonpotable protocol may result in reduced L. pneumophila detection due to the pretreatment step and the smaller volume of sample tested.
Sodium thiosulfate must be utilized when collecting a chlorinated sample. Sodium thiosulfate does not need to be present when collecting a non-chlorinated sample, but if it is present, will not have an adverse impact on the Legiolert test results.
Sample dilutions and QC/PTs must be prepared in sterile containers without sodium thiosulfate.
Both the 100 mL and 10 mL protocols have been validated to detect L. pneumophila in potable water. The 100 mL protocol has a lower limit of detection but requires the use of a supplement before the Legiolert reagent is added. Laboratories should choose between the 100 mL and 10 mL protocols based on their limit of detection and workflow requirements.
The Legiolert test detects L. pneumophila in potable and nonpotable water samples. This test is based on a bacterial enzyme-detection technology that signals the presence of L. pneumophila through utilization of a substrate present in the Legiolert reagent. L. pneumophila cells grow rapidly and reproduce using the rich supply of amino acids, vitamins, and other nutrients present in the Legiolert reagent. Actively growing strains of L. pneumophila use the added substrate to produce a brown color indicator.
L. pneumophila causes the overwhelming majority of Legionnaires’ disease worldwide. Waterborne, non-pneumophila Legionella causes less than 2% of Legionnaires’ disease in almost every country that tracks cases. A test that is more sensitive to L. pneumophila better protects public health than traditional methods of detecting Legionella. Not only do traditional, plate-based methods only recover certain Legionella species, they have demonstrated low recovery, low sensitivity, and a high rate of false negativity.23-25
The detection limit of the Legiolert test depends on the protocol used:
100 mL protocol for potable water: <1 organism/100 mL
10 mL protocol for potable water: <10 organisms/100 mL
1 mL protocol for nonpotable water: <100 organisms/100 mL
Legiolert Supplement is only required to be used when testing an undiluted 100 mL potable water sample. With 100 mL potable samples, the hardness level must be checked, and the appropriate volume of supplement must be added. Note that supplement will be added regardless of the level of hardness; the results of the hardness testing determine how much supplement is added. Refer to the product insert for specific procedures. No sample types other than undiluted 100 mL potable samples require the use of Legiolert Supplement.
The hardness of the water sample can impact the Legiolert test, the supplement adjusts hardness to ensure proper functioning of the test when using the undiluted 100 mL potable protocol.
Any wells with a brown color and/or turbidity are positive for L. pneumophila. No other colors are positive for L. pneumophila.
Potable water samples are incubated at 39°C (± 0.5°C) for 7 days. Nonpotable water samples are incubated at 37°C (± 0.5°C) for 7 days. Maintaining these temperatures is critical to the functioning and success of the test. L. pneumophila is more thermoresistant than other bacteria found in water, and the increased temperature acts as a selective agent. For this reason, trays cannot be removed completely from incubator prior to final read.
Results can be read any time on the 7th day.
No. Controlled, uninterrupted incubation temperature is a critical part of the Legiolert method. False-positive results due to bacteria other than L. pneumophila and/or reduced L. pneumophila detection can occur at temperatures other than 39°C (± 0.5°C) for potable samples and 37°C (± 0.5°C) for nonpotable samples. Because L. pneumophila is more thermoresistant than other bacteria, maintaining these temperatures is critical to ensuring the selectivity of the Legiolert test.
The Legiolert test requires a humidity level that ensures ≤15% sample volume loss in the Quanti-Tray/Legiolert wells. Appropriate humidity can typically be achieved by incubating Quanti-Tray/Legiolert in a container that traps moisture. For example, a large plastic bag could be used for several Quanti-Tray/Legiolert samples. Alternatively, humidity may be maintained by placing a pan of water on the bottom of the incubator so that it covers approximately 80% of the bottom interior surface.
Yes, if the results are positive. An inoculated Legiolert test sample that is positive before 7 days is a confirmed positive test for L. pneumophila. However, for an accurate quantitative determination of L. pneumophila in a sample, the results should be read at 7 days. Do not remove trays completely from incubator prior to final read, as deviations in temperature during incubation may cause false positive results.
Yes, if the results are negative. If an inoculated Legiolert test sample is inadvertently incubated for more than 7 days, the lack of brown color and turbidity is a valid negative test result. However, brown color and/or turbidity that develops after 7 days is not a valid positive test result; the test should be repeated or verified.
Store the Legiolert test at 2–25°C away from light and humidity.
Check with your local, state, and/or federal authorities for proper disposal of biohazard materials at your facility.
L. pneumophila ATCC 33152 (WDCM 00107) or ATCC 33156 (WDCM 00180) are recommended positive control strains. Enterococcus faecalis ATCC 29212 (WDCM 00087) is a recommended negative control strain. Additionally, IDEXX offers IDEXX-QC Legionella pneumophila (catalog number WQC-LP). Please contact your IDEXX representative for ordering information.
Yes, the Binder incubator available from IDEXX Water is able to handle the higher humidity required by the Legiolert Test. Appropriate humidity can typically be achieved by placing a pan of water on the bottom of the incubator so that it covers approximately 80% of the bottom interior surface. Appropriate humidity can also be achieved by incubating Quanti-Tray/Legiolert in a container that traps moisture. For example, a large plastic bag could be used for several Quanti-Tray/Legiolert samples.
Nonpotable water may contain high concentrations of bacteria other than L. pneumophila. The Legiolert test nonpotable protocol and the Legiolert Pretreatment have been optimized to prevent these non-target organisms from interfering with the test result.
Resources & Tools
Tests & Accessories
Accuracy matters when it comes to public health.
Search the Water Tests & Accessories tool
Product Information
Legiolert Test (20-test pack)
Product Number: 98-0002710-00
Catalogue Number: WLGT-20
Legiolert Test (100-test pack)
Product Number: 98-0005738-00
Catalogue Number: WLGT-100
Legiolert Pretreatment
Product Number: 98-0007740-01
Catalogue Number: WLGT-PRE
Legiolert Supplement
Product Number: 98-0005745-01
Catalogue Number: WLGT-SUP
Quanti-Tray/Legiolert (20 pack)
Product Number: 98-0005796-00
Catalogue Number: WQTLGT-20
Quanti-Tray/Legiolert (100 pack)
Product Number: 98-0005754-00
Catalogue Number: WQTLGT-100
IDEXX-QC Legionella pneumophila Kit
Product Number: 98-0009287-01
Catalogue Number: WQC-LP
Resources
IDEXX Water has reference materials and approval documents to support the many products in our water portfolio. Find the document(s) you need by selecting the link below.
Search the Reference & Regulatory Documents tool
Water Customer Support
UK Headquarters
IDEXX Technologies Ltd Units 1B - 1D
Newmarket Business Park
Studlands Park Avenue
Newmarket, Suffolk, CB8 7ER
Tel: +44 (0) 1638 676800
wateruk@idexx.com
Water International
Australia
Brazil
Canada
China
France
Germany
Italy
Japan
Latin America
Spain
Taiwan
United Kingdom
ISO Certifications
*The Legiolert Test is intended to be used only for water quality research and analysis, by technically qualified individuals or under their supervision.
References
- Barrette I. Comparison of Legiolert and a conventional culture method for detection of Legionella pneumophila from cooling towers in Québec. J AOAC Int. 2019;102(4):1235–1240. doi:10.5740/jaoacint.18-0245
- Boczek LA, Tang M, Formal C, Lytle D, Ryu H. Comparison of two culture methods for the enumeration of Legionella pneumophila from potable water samples. J Water Health. 2021;19(3):468–477. doi:10.2166/wh.2021.051
- Checa J, Carbonell I, Manero N, Martí I. Comparative study of Legiolert with ISO 11731-1998 standard method-conclusions from a Public Health Laboratory. J Microbiol Methods. 2021;186:106242. doi:10.1016/j.mimet.2021.106242
- Inoue H, Baba M, Tayama S. Evaluation of Legiolert for quantification of Legionella pneumophila from bath water samples. Biocontrol Sci. 2020;25(3):179–182. doi:10.4265/bio.25.179
- Matthews S, Trigui H, Grimard-Conea M, Vallarino Reyes E, Villiard G, Charron D, Bédard E, Faucher S, Prevost M. Detection of Diverse Sequence Types of Legionella pneumophila by Legiolert Enzymatic-Based Assay and the Development of a Long-Term Storage Protocol. Microbiol Spectr. 2022;10(6):e0211822. doi: 10.1128/spectrum.02118-22.
- McCuin RM, Bartrand TA, Clancy JL. Legionella pneumophila recovery using Legiolert and a traditional culture method. AWWA Water Sci. 2021;3(3):e1228. doi:10.1002/aws2.1228
- Monteiro SN, Robalo AM, Santos RJ. Evaluation of Legiolert for the detection of Legionella pneumophila and comparison with spread-plate culture and qPCR methods. Curr Microbiol. 2021;78(5):1792–1797. doi:10.1007/s00284-021-02436-6
- Petrisek R, Hall J. Evaluation of a most probable number method for the enumeration of Legionella pneumophila from North American potable and nonpotable water samples. J Water Health. 2018;16(1):25–33. doi:10.2166/wh.2017.118
- Rech MM, Swalla BM, Dobranic JK. Evaluation of Legiolert for quantification of Legionella pneumophila from non-potable water. Curr Microbiol. 2018;75(10):1282–1289. doi:10.1007/s00284-018-1522-0
- Sartory DP, Spies K, Lange B, Schneider S, Langer B. Evaluation of a most probable number method for the enumeration of Legionella pneumophila from potable and related water samples. Lett Appl Microbiol. 2017;64(4):271–275. doi:10.1111/lam.12719
- Scaturro M, Buffoni M, Girolamo A, et al. Performance of Legiolert Test vs. ISO 11731 to confirm Legionella pneumophila contamination in potable water samples. Pathogens. 2020;9(9):690. doi:10.3390/pathogens9090690
- Spies K, Pleischl S, Lange B, et al. Comparison of the Legiolert/Quanti-Tray MPN test for the enumeration of Legionella pneumophila from potable water samples with the German regulatory requirements methods ISO 11731-2 and ISO 11731. Int J Hyg Environ Health. 2018;221(7):1047–1053. doi:10.1016/j.ijheh.2018.07.006
- Association française de normalisation (AFNOR). Attestation n° IDX 33/06-06/19. 2019. Available from https://nf-validation.afnor.org/wp-content/uploads/2019/09/Synt-33-06-06-19_en.pdf
- Centers for Disease Control and Prevention. Table 1, Waterborne disease outbreaks associated with treated recreational water and untreated recreational water, by year and jurisdiction—waterborne disease and outbreak surveillance system, United States, 2011–2012. www.cdc.gov/healthywater/surveillance/recreational/2011-2012-tables.html. Updated March 28, 2018. Accessed September 14, 2018.
- Centers for Disease Control and Prevention. Table 1, Waterborne disease outbreaks associated with treated recreational water or untreated recreational water, by year and jurisdiction—waterborne disease and outbreak surveillance system, United States, 2013–2014. www.cdc.gov/healthywater/surveillance/recreational/2013-2014-tables.html. Updated May 16, 2018. Accessed September 14, 2018.
- Centers for Disease Control and Prevention. Outbreaks associated with environmental and undetermined water exposures—United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 64(31);849-851. www.cdc.gov/MMWR/preview/mmwrhtml/mm6431a3.htm. Accessed September 14, 2018.
- Centers for Disease Control and Prevention. Waterborne disease outbreaks associated with environmental and undetermined exposures to water—United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 66(44);1222-1225. www.cdc.gov/mmwr/volumes/66/wr/mm6644a4.htm. Accessed September 14, 2018.
- Centers for Disease Control and Prevention. Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 64(31);842-848. www.cdc.gov/mmwr/preview/mmwrhtml/mm6431a2.htm. Accessed September 14, 2018.
- Centers for Disease Control and Prevention. Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 66(44);1216--1221. www.cdc.gov/mmwr/volumes/66/wr/mm6644a3.htm. Accessed September 14, 2018.
- Surveillance report: Legionnaires’ disease in Europe (Years 2009-2015). Stockholm, Sweden: European Centre for Disease Prevention and Control; published 2011-2017.
- Centers for Disease Control and Prevention. Outbreaks associated with environmental and undetermined water exposures—United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 64(31);849-851. www.cdc.gov/MMWR/preview/mmwrhtml/mm6431a3.htm. Accessed September 14, 2018.
- Centers for Disease Control and Prevention. Toolkit for Controlling Legionella in Common Sources of Exposure. https://www.cdc.gov/legionella/downloads/Control-Toolkit-All-Modules.pdf
- Lucas CE, Taylor, TH, Jr, & Fields, BS. Accuracy and precision of Legionella isolation by US laboratories in the ELITE program pilot study. Water research, 2011:45(15), 4428–4436. doi:10.1016/j.watres.2011.05.030
- Díaz-Flores Á, Montero JC, Castro FJ, Alejandres EM, Bayón C, Solís I, Fernández-Lafuente R, & Rodríguez G. Comparing methods of determining Legionella spp. in complex water matrices. BMC microbiology 2015:15, 91. doi:10.1186/s12866-015-0423-7
- Boulanger CA, Edelstein PH. Precision and accuracy of recovery of Legionella pneumophila from seeded tap water by filtration and centrifugation. Appl Environ Microbiol. 1995 May;61(5):1805-9. doi: 10.1128/aem.61.5.1805-1809.1995.
- Borges A, Simões M, Martínez-Murcia A, Saavedra MJ. Detection of Legionella spp. in Natural and Man-made Water Systems Using Standard Guidelines. Journal of Microbiology Research. 2012:2(4), 95-102. doi: 10.5923/j.microbiology.20120204.06